Researchers at the Duke Human Vaccine Institute have led an effort to develop a more accurate way to gauge the incidence of HIV infections in large populations, which will improve research and prevention strategies worldwide.
The new method more correctly identifies new vs. long-standing infections – an important distinction for determining where to target public health measures and research, and for evaluating whether interventions are successful at reducing HIV transmission.
“Recent advances — including effective anti-retroviral drugs that both treat and prevent HIV infections — have changed the landscape in the HIV field,” said senior author Georgia Tomaras, Ph.D., professor in the Department of Surgery and director of research at Duke Human Vaccine Institute. The study is published online Dec. 21 in the journal JCI Insight.
“Improved methods for classifying recent infection from older infections are critically needed to help identify the most effective prevention strategies,” Tomaras said.
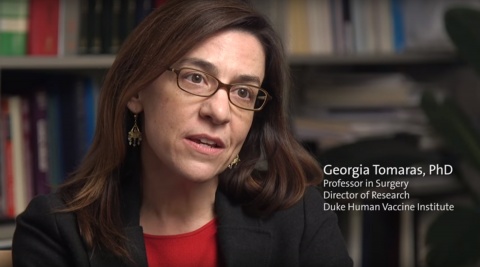
Tomaras and colleagues worked to develop a way to measure HIV incidence that takes into account the unique features of the current epidemic while also capitalizing on recent insights into how the virus and the body interact during the early phases of infection.
The result was an assay that identifies new combinations of naturally occurring antibody biomarkers, resulting in a promising set of four biomarkers that could be used. The new assay has a longer, and thus more accurate, time-period that constitutes recent infection, and fewer false classifications.
“Having a more accurate HIV incidence test could substantially reduce costs for researchers, because they would need a much smaller sample size to enroll in studies,” Tomaras said.
“Additionally, from a public health standpoint, a more accurate HIV incidence test would help identify hot spots of recent infections, so that prevention efforts could be better targeted to where outbreaks are happening,” said Kelly Seaton, Ph.D., lead author on the study.
In addition to Tomaras and Seaton, study authors include Nathan A. Vandergrift, Aaron W. Deal, Wes Rountree, John Bainbridge, Eduard Grebe, David Anderson, Sheetal Sawant, Xiaoying Shen, Nicole L. Yates, Thomas N. Denny, Hua-Xin Liao, Barton F. Haynes, Merlin L. Robb, Neil Parkin, Breno R. Santos, Nigel Garrett, Matthew A. Price, Denise Naniche, Ann C. Duerr, the CEPHIA group; Sheila Keating, Dylan Hampton, Shelley Facente, Kara Marson, Alex Welte, Christopher D. Pilcher and Myron S. Cohen.
This work received support from the Bill & Melinda Gates Foundation (OPP1068333, OPP1062806, OPP1115799, and OPP1017716) and the Collaboration for AIDS Vaccine Discovery, Vaccine Immune Monitoring Center (OPP1032144, OPP1146996). Additional support was provided by the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health, the Duke Center for AIDS Research Immunology Core (AI064518), the Center for HIV/AIDS Vaccine Immunology (CHAVI grant AI067854), and the Duke Center for HIV/AIDS Vaccine Immunology and Immunogen Discovery (CHAVI-ID grant AI067854); and the U.S. Military HIV Research Program through a cooperative agreement between the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. and the U.S. Department of Defense.
















