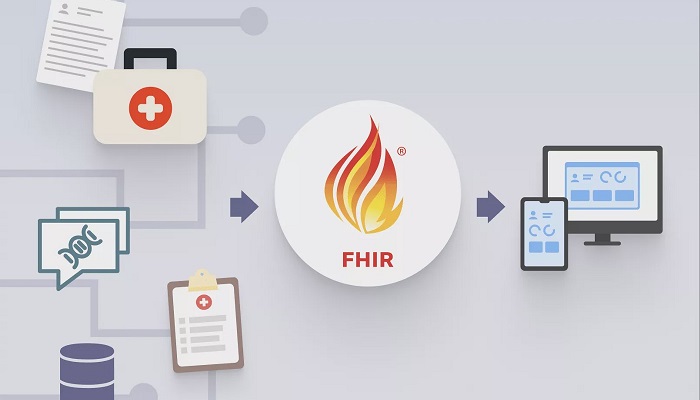
Most electronic health record systems can provide data to FHIR apps, enabling secure information transfer when and where it is required. Fast Healthcare Interoperability Resources, or FHIR (called Fire), standardises how healthcare data is shared between various computer systems, independent of how the data is kept in these systems.
Through the FHIR interface, FHIR apps ingest data. Health information can be exchanged between doctors and patients, as well as between clinicians and healthcare systems, using the worldwide interoperability standard. FHIR may appear to be a complicated technical idea, yet patients, clinicians, and healthcare systems can apply it in everyday situations.
It improves access to health information for patients as well as for professionals, according to Dr. Schleyer. The ability to extract data from an electronic health record and perform meaningful tasks with it, such as analyse patterns, offer clinical decision assistance, or handle a specialised area not handled by a commercial electronic medical record system, is actually the fundamental competency of many FHIR apps.
Charles Jaffe, M.D., PhD, a co-author on the paper, said that the publication of this widely collaborative work represents a key step in stressing the significant international effort toward the adoption of HL7 FHIR. They see this platform as a crucial resource for the growing community of end users as well as technical implementers as the use of FHIR for patient care and research spreads. The Chief Executive Officer of HL7 is Dr. Jaffe. The new study, which was just published in JAMIA Open, highlights the quick growth and adoption of free and user-friendly FHIR apps over the course of less than a decade and predicts even faster growth and adoption in the future.
112 apps were examined to gauge the FHIR app landscape. 45 were devoted to research, and 74 to clinical treatment. A larger percentage were standalone web-based applications, whereas a smaller percentage were embedded within electronic health records.
The majority of the clinical apps were used in various healthcare settings, underscoring, in the authors’ opinion, the flexibility of FHIR. Instead of being designed with patients in mind, the majority of apps were created by software companies. Dr. Schleyer explained that when addressing FHIR, they were discussing a cutting-edge method of safely exchanging health data from various information systems.
FHIR can be compared to the electrical plug in the home as a plug-and-play standard. Electricity flows when people plug something into an outlet, and the TV or other item turns on without our being concerned about what the plug does. The same is true with FHIR. This new standard enables access to information across systems.
According to the 21st Century Cures Act, patient-facing FHIR apps are necessary for electronic health record certification in the United States. The Centers for Medicare and Medicaid Services (CMS) will start mandating that payers adopt FHIR apps in 2023 for a variety of use cases. The implementation of FHIR-based personal health records and information sharing with providers are the main objectives of the European Union’s InteropEHRate and India’s Digital Health Blueprint. National patient identification systems are accessible via FHIR through the Ministry of Health of New Zealand and the National Health Service of the United Kingdom.