Accenture study explores the future of integrated healthcare delivery Nations around the world are making significant efforts to adopt healthcare information technology as a path toward “connected health.”
The goals are straightforward enough –higher quality, more accessible and cost-effective healthcare – but the path there is intricate and varied. Accenture has released a comprehensive new report, Connected Health: The Drive to Integrated Healthcare Delivery, which takes an in-depth look at the progress toward connected health in eight countries. The study identifies the key dynamics, challenges and lessons guiding each country along its unique journey to more integrated healthcare delivery. Accenture’s connected health study combines deep research – including interviews with more than 160 healthcare leaders, a survey of more than 3,700 doctors and clinicians, case studies, literature reviews and more – and delivers a broad analysis of how health systems in these countries can accelerate progress and realize tangible benefits from their initiatives.

What does it mean?
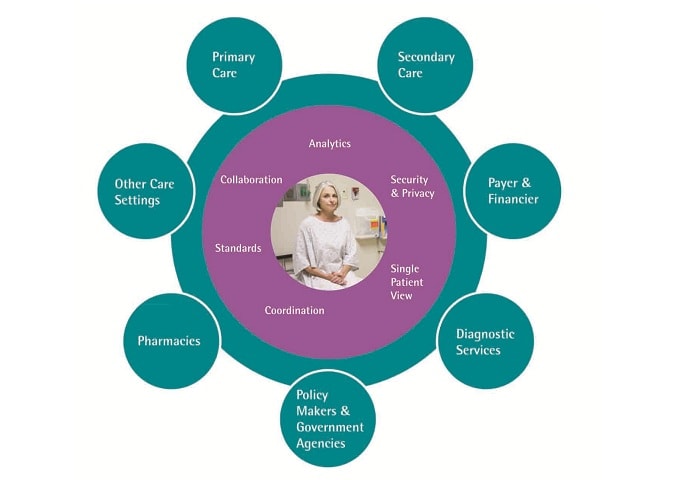
Connected health: Healthcare delivery that leverages the systematic application of healthcare IT to facilitate the accessing and sharing of information, as well as subsequent analysis of health data across healthcare systems. Connected health encourages communication and collaboration among all of the various stakeholders involved in a patient’s health. It uses knowledge and technology in new ways for more effective, efficient and affordable healthcare.
Healthcare IT: The umbrella framework to describe the comprehensive management of health information across computerized systems and its secure exchange between consumers, providers, government and quality entities,and insurers.
Electronic Medical Record (EMR): A computerized medical record created in an organization that delivers care, such as a hospital or physician’s office, usually part of a local standalone health information system that allows storage, retrieval and modification of records.
Electronic Health Record (EHR): A systematic collection of electronic health information about inpidual patients or populations in digital format and capable of being shared across different healthcare settings Health Information.
Exchange (HIE): The mobilization of healthcare information electronically across organizations within a region, community or hospital system.
What is Connected health?
The world is facing unprecedented health challenges – steadily rising costs and budget pressures, aging populations, rising chronic disease rates and growing expectations for more convenient, affordable, highquality and personalized care. Add to the mix the simple fact that people are living longer – by some estimates, 50 percent of people born today will live to 100 – and increasing chronic obesity rates directly contribute to rising healthcare costs. These challenges highlight the need for a complete transformation of healthcare—one that that is integrated across the entire continuum of care and can offer a more sustainable health system in the twenty-first century and beyond.Integrated healthcare delivery relies on a key enabler—what Accenture calls “connected health.” Connected health means systematically applying healthcare information technology to facilitate the accessing and sharing of information, and to enable the subsequent analysis of health data across healthcare systems. (In concert with that, integrated care refers to the delivery of healthcare.)
But connected health goes beyond simply managing and analyzing patients’ clinical data. It encourages communication and collaboration among all the stakeholders involved in a patient’s health to get to improved care – and better health outcomes – at lower costs. Though there are clearly differences among the countries in the study, Accenture’s research shows that these countries have a vision for connected health, and there are commonalities in their responses to the growing health crisis.
To improve quality and access while getting a grip on costs, they are all moving toward integrated healthcare to some degree. The approaches range from “topdown,” governments looking at the whole system to develop nationwide solutions, to “bottom-up,” leaving leadership to local jurisdictions and inpidual healthcare professionals. Between these two approaches is a “middle-out” strategy, in which a central government provides an overarching direction but allows the solutions to develop locally.m.
The research revealed that all eight countries in the study—Australia, Canada, England, France, Germany, Singapore,Spain and the United States—have started the journey,which Accenture categorizes into three overlapping stages:The Connected Health Ecosystem
1. Healthcare IT adoption — designing the digital infrastructure to be able to capture health data.
2. Health information exchange (HIE) — exchanging health information between clinicians, across administrative groups and with patients.
3. Insight driven healthcare — using advanced analysis of data to better inform clinical decision-making, population health management and new care delivery models.
Key findings from Accenture’s connected health study
• Connected health is a must. Governments around the world see connected health as a critical and essential means to improve citizens’ access to quality, lower-cost healthcare. Connected health has gained a high level of acceptance, and there is a prevailing view that without a solid connected health platform, it will be difficult to meet today’s—and future—health challenges.
• Integration is possible. Connected health can and will work with deep and varying underlying industry structures. Different countries have very different provider systems, and these are unlikely to change in the near term. All are fragmented, but in different ways. Healthcare IT connectivity helps bridge this fragmentation to provide better integration.
• Connected health is on a self-sustaining path. Quality and performance measures require an integrated look at the data.These measures also increase the need for healthcare IT, and process change to enable such measures.
Measuring progress
To make their way along the three stages, most doctors are changing at least some of their methods.This has largely been thanks to the introduction of new healthcare information technology, a broad range of solutions, including elements such as electronic medical records (EMR) and HIE. A key component of the Accenture connected health study is a survey of more than 3,700 physicians in the eight countries, which measured their use and the perceived benefits of healthcare IT. Based on the findings, Accenture compared each country’s progress in two important stages of the connected health journey – healthcare IT adoption and HIE.
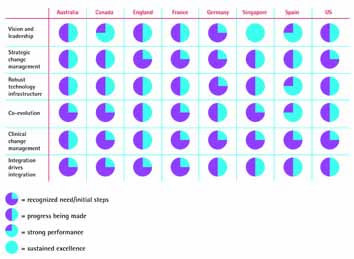
The chart shows two important elements of connected health: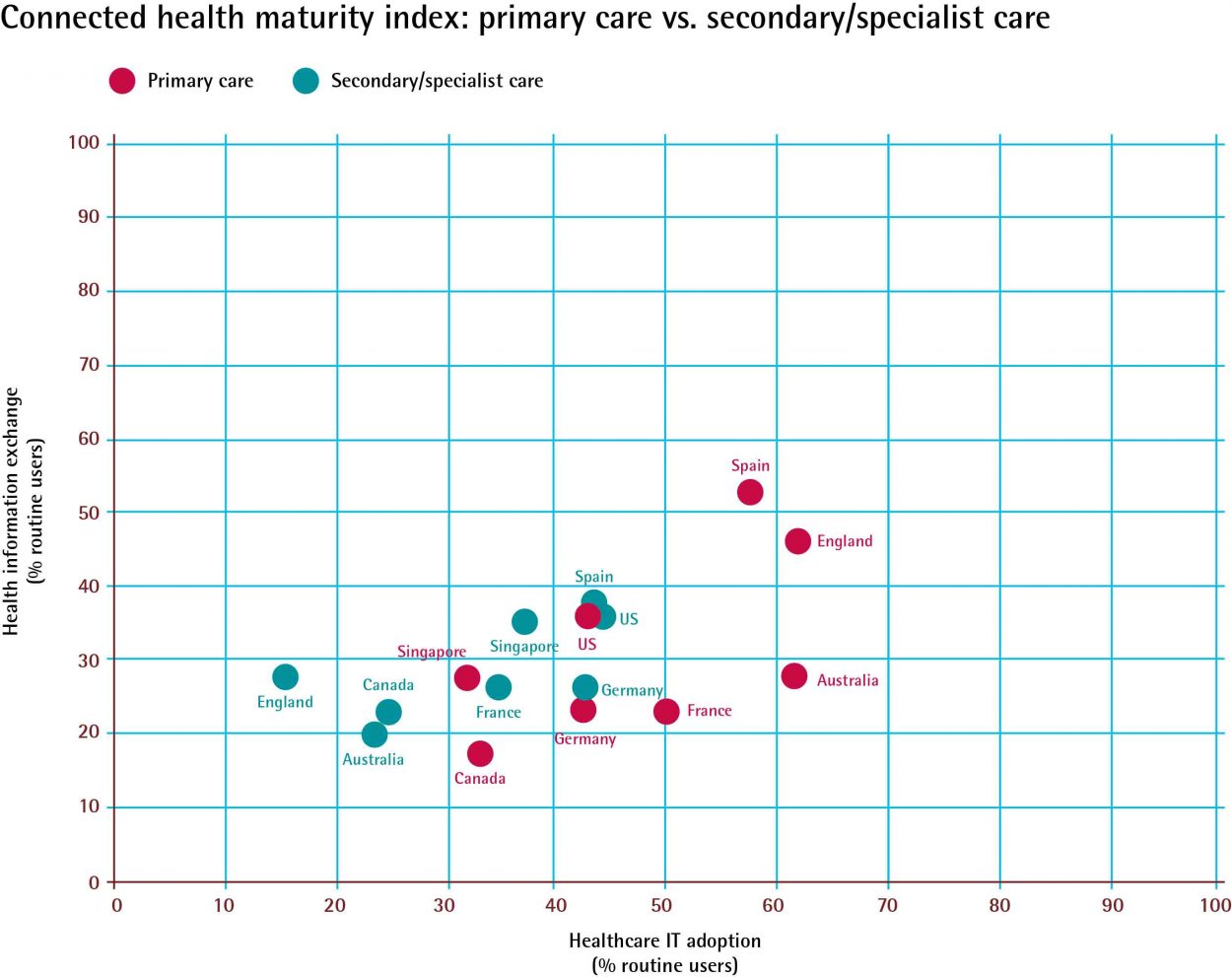
Progress toward health information technology adoption and progress toward health information exchange. The horizontal axis is based on how physicians are using four key health IT functionalities within their practices: administrative tools, electronic patient notes, electronic alerts/ reminders and computerized decision support systems. The analysis on the vertical axis is based on physicians’ use of seven key HIE functionalities to connect with other clinicians: electronic communications, e-notifications, e-referrals, e-access to clinical data about patients who see a different provider, e-prescribing and receipt of clinical results to populate patients’ EMRs and electronic order requests. As the chart demonstrates, while all countries are making progress in the adoption of healthcare IT, some are more advanced than others.
But most countries in Accenture’s survey lag behind world leaders such as Denmark, Sweden and New Zealand. In these three countries, nearly all primary care physicians use EMR, generally defined as computerized medical data that hospitals or physicians create to track patients’ health. These countries also demonstrate use of electronic health records (EHR), commonly defined as a digital file capable of being shared across different healthcare settings and may include such information as demographics, medical history, medications, immunization status, lab results, radiology images, vital signs and billing information. (An EMR is typically part of an EHR solution or platform). The overall picture in both primary and secondary care shows most of the countries are still at a relatively early stage of the connected health journey.
Some—such as Spain and England— are further along, particularly in primary care, while others—such as Canada, France and Germany—are at an earlier stage in their journey.
• Spain has adopted EMR broadly and enjoys a high level of healthcare IT adoption across many of its regions, with the challenge of implementing these practices consistently across all regions and achieving national interoperability.
• England has seen significant improvements in its IT and communications infrastructure over the last few years, including a picture archiving and communication system (PACS) and patient records transfer.
• The US’s healthcare IT picture has been inconsistent across different states, networks and care settings.
• Singapore has more advanced healthcare IT and HIE in the public setting, with its National Electronic Health Record available to a number of public sector providers including acute hospitals, polyclinics and community hospitals.
• Australia’s healthcare IT adoption is particularly advanced in primary care settings, and recent investments in a national PCEHR program are expected to drive greater progress across the country.
• Healthcare IT adoption in Canada across primary and secondary care is limited, but a common architecture has been agreed to and the country is working toward pan-Canadian EHR. Meanwhile, HIE adoption is nascent but growing.
• France offers a mixed picture in healthcare IT adoption, with large urban regions making faster progress than rural and sparsely populated regions.

• Germany has widespread use of healthcare IT within primary and secondary care settings, but it’s mainly focused on administrative,rather than clinical, processes. Obstacles along the path to connected health Another key component of the Accenture connected health study is a series of interviews with more than 160 health system leaders across the eight countries. From those interviews, the message was clear: although there is progress toward connected health, it’s not happening as quickly as many stakeholders would like. A number of challenges are hindering this progress, and they fall into four categories:
1. Systems and policies – including a lack of clear strategies linking healthcare IT investment to health outcomes, poor financial incentives, fragmented healthcare delivery and a lack of interoperability standards.
2. Organization and management – including financial constraints on investment, a lack of credible business cases, high costs, poor collaboration between organizations, technical limitations and substandard project management.
3. Clinicians and end users—including physician resistance to technology and practices that slow their productivity, increase overhead costs, introduce information with no clinical benefit or raise legal liability.
4. Patients and the public—including concerns over privacy and data security, lack of regulatory oversight and the need to encourage people to play a bigger role in managing their own health. Accenture asked physicians surveyed to list their top five barriers for healthcare IT adoption and HIE. Among their top concerns were: IT systems that can’t ‘talk’ to each other;concerns about privacy and security of data; cost of the systems to their organization; loss of productivity or excessive time spent inputting data; and lack of financial incentives for adoption. These challenges will have to be addressed if governments and health organizations are to speed their connected health progress. Realizing the benefits The Accenture study yielded evidence of the benefits from healthcare adoption and from the systemwide exchange of data. It shows that connected health facilitates care coordination and integration, disease management, reduction of clinical errors and the use of care protocols and clinical practice guidelines, as well as providing opportunities for administrative and clinical cost savings.
There are specifically three clear levels of value creation, from early, relatively small returns to producing value through care transformation.
• Clinical efficacy. These include reducing administrative activities and costs, eliminating duplicate lab and radiology tests, improving patient safety through 24/7 access to comprehensive, legible medical records and speeding up access to patient medical histories and vital information at the point of care to improve the patient experience and support clinical decisionmaking.
• Shared knowledge. Deepening HIE and connectivity can help reduce medical errors and improve care quality, with benefits such as drug interaction alerts, sophisticated tools to enhance clinical decisionmaking through evidence-based care protocols, and innovations and new capabilities in population care which increase the potential for preventative and low-cost care for chronic conditions.
• Care transformation. Advanced analytics can inform clinical decision making, population health management and the creation of new care delivery models, including patient self-management and better coordination across settings.
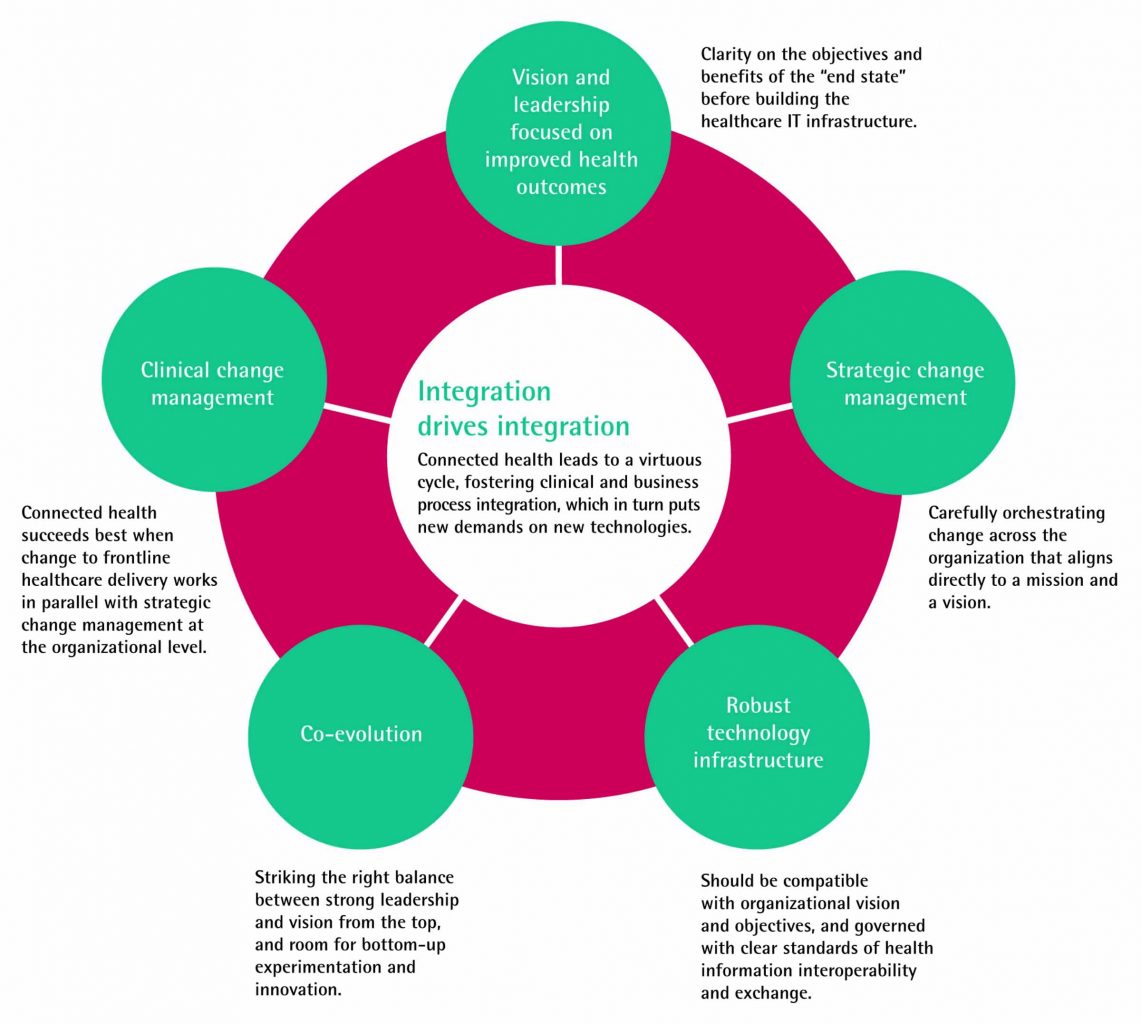 Navigating the journey – the six dynamics that characterize success The journey to connected health is hardly easy, but those that have started down the path provide valuable lessons. In its study, Accenture identified six key dynamics that systems and organizations must employ to lay a solid foundation for connected health.
Navigating the journey – the six dynamics that characterize success The journey to connected health is hardly easy, but those that have started down the path provide valuable lessons. In its study, Accenture identified six key dynamics that systems and organizations must employ to lay a solid foundation for connected health.
1. Vision and leadership focused on improved health outcomes Connected health is a means to an end. Health providers, governments and other key players must be clear on the objectives and benefits of the “end state” before building the healthcare IT infrastructure. Connected health must be part of a clear vision about improved quality, enhanced access to care and better control of costs,which all stakeholders understand and embrace.
2. Strategic change management Connected health is not simply a tactical intervention in an organization or system. Developing connected health means carefully orchestrating change across the organization that aligns directly to a mission and a vision. This transformation should have a strong positive impact on culture, management and clinical systems, behavior and patientprovider- payer interactions, well beyond the changes required by technology alone.
3. Robust technology infrastructure Connected health must be built on the back of a robust healthcare IT infrastructure. This infrastructure should be compatible with organizational vision and objectives, and governed with clear standards of health information interoperability and exchange. Without a coherent healthcare IT architecture expressly designed to ensure interoperability, systems may apply ad hoc solutions, which typically fail to show healthy returns on investment. Healthcare IT infrastructures must also be flexible enough to adapt as the needs, demands and aspirations of citizens, clinicians
and health managers change.
4. Co-evolution In developing connected health, organizations have to strike the right balance between strong leadership
and vision from the top, and room for bottom-up experimentation and innovation. Global experience demonstrates that top-down approaches alone fail to build clinical buy-in, and bottom-up approaches alone seldom achieve system-wide interoperability—both of which are key to success. Learning from those local solutions and disseminating best practice across the organization or system will help to ensure wider adoption, where appropriate.
5. Clinical change management Connected health succeeds best when change to frontline healthcare delivery works in parallel with strategic change management (the second dynamic) at the organizational level. Sophisticated analytics can identify needs for change and drive business intelligence and provide statistical evidence that can help reshape clinical decision-making and healthcare protocols. However, analytics alone is not enough to effect change. Without a strong framework of clinical governance, peer review and performance management across the system, clinical changes can be fragmented, disruptive and inefficient.
6. Integration drives integration Connected health leads to a virtuous cycle, fostering clinical and business process integration, which, in turn, puts new demands on new technologies. This requires organizations to put in place project management processes that orchestrate the five dynamics listed above, and to continually reassess their role, what services they provide and the need to develop, extend and connect those services. There is very little room to integrate different levels of care if each organization or system is disconnected. Where each country stands 14 | Making the Case for Connected Health www.accenture.com/
While the overall picture in connected health shows most of the eight countries in the study are still at a relatively early stage of the journey, some are further advanced than others in each of the six dynamics. Moving forward on the journey: Together, one step at a time Taking the first steps on a connected health journey requires careful assessment, planning and preparation. Wherever a healthcare system may be in its current healthcare IT development, the challenges it faces depend on its unique combination of national, regional and health system factors. It is crucial to have a clear appreciation of how the barriers and challenges in each country will affect its progress toward connected health. One of the important lessons from the study is that “biting off more than you can chew” can result in failure.
The “bite-size” chunks that healthcare leaders in Singapore are embracing, for example, and the “chunkability” in some of the more successful national and system-wide initiatives, should encourage those who recognize that the journey for ward is best taken one step at a time. Overly ambitious plans—especially if organizations undertake them without establishing a shared sense of ownership—can be a mistake. Incremental gains build understanding, helping support and provide the foundations for continued development and progress.
There are four particular areas of continuing growth and evolution that are critical to transform a health system:
• Developing integrated systems that blend EMR with new methods of communication, remote care and process management to build seamless systems and workflows. There are, for example, new clinician and patient interfaces under development that will make healthcare data and analytical tools easier to access, navigate and put to good use, and natural language processing and voice recognition technologies are being developed that can instantly digitize healthcare consultations and integrate them into EMR systems.
• Redirecting healthcare interventions away from expensive hospital settings and into people’s homes through telemedicine,
remote care and mobile health. A whole new range of applications— from handheld devices to facilitate remote diagnosis to touchscreen technologies and “smart” devices (such as “intelligent shirts” that use electrodes and sensors to monitor patients’ vital signs, activity sensors and webcams) –will enable remote monitoring and communication.
• Transforming the role of patients in managing their own wellbeing through shared decision-making, condition monitoring and chronic disease management. New, independently developed, mobile healthcare apps are giving people the tools to educate themselves on how to eat well and live well, while personal health records (PHRs) and patient portals help them to manage their own care needs.
• Exploring the potential of genomics to personalize treatment and wellness plans, present clinicians with a powerful range of analytical and diagnostic tools, and enable managers to coordinate care, target resources and improve public health outcomes. Among other benefits, this will help identify early – even preventative – interventions where patients have a genetic predisposition to certain medical conditions. Connected Health: The Drive Toward Integrated Healthcare Delivery points to a future in which organizations – and entire countries – can achieve integrated healthcare and improved health outcomes through the power of healthcare IT and the functional benefits of health information exchanges. Connected health helps drive integration and innovation, and the future prospects of each are more compelling and more valueproducing—if also more challenging— than the status quo. By developing and harnessing the value of connected health, leaders around the world are poised to shape the future, to lead a journey toward high performance and improved health outcomes—for themselves, their organizations, their patients and their countries.