Hospital acquired infections have become so commonplace that patient horror stories have lost the power to shock.No hospital — not even the cleanest, most advanced healthcare facility — is immune to this epidemic or can ignore its twin crisis: the dramatic rise of antibiotic-resistant “superbugs.”
Already, 70% of bacteria worldwide have developed resistance to antibiotics, making treatment of serious infections increasingly difficult and less successful.
“Far too many patients are getting infected with dangerous, drug-resistant bacteria in healthcare settings,” Tom Frieden, M.D., M.P.H., director of the U.S. Centres for Disease Control and Prevention has warned. “Doctors and healthcare facilities have the power to protect patients – no one should get sick while trying to get well.”
And yet, each year millions do.
On any given day, an estimated 1.4 million hospitalized patients around the world have at least one healthcare associated infection. Pneumonia, meningitis, colitis, gastroenteritis, peritonitis, sepsis — the list is long. Compared to other patients, research shows, infected patientsare80% more likely to die within 90 days.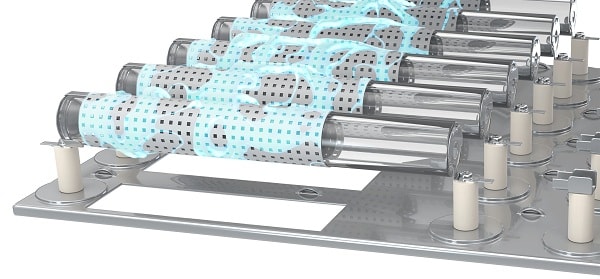 Each year, hospital pathogens infect 6 million patients in Europe and the United States and are responsible for 140,000 deaths. In the United States, the number of deaths attributed to hospital acquired infections, 99,000, is more than twice the number of people who die each year in car accidents.
Each year, hospital pathogens infect 6 million patients in Europe and the United States and are responsible for 140,000 deaths. In the United States, the number of deaths attributed to hospital acquired infections, 99,000, is more than twice the number of people who die each year in car accidents.
Even in high-income countries, infections strike 5% to 10% of hospitalized patients and an alarming 30% of patients in intensive care units.In developing countries, the crisis is more acute; as the World Health Organization (WHO) notes, the childhood death rate from hospital acquired infections equates to “a plane crashing every hour.”
For hospitals, the costs are staggering.
Patients who acquire infections from surgery spend, on average, an additional 6.5 days in the hospital and are five times more likely to be readmitted after discharge.Those infected by a superbug, may spend an additional 16.9 days in the hospital.A single central-line associated bloodstream infection costs $45,814. Onemethicillin-resistant Staphylococcus aureus (MRSA) infection in the neonatal intensive care unit can extend the infant`s hospital stay by 40 days, at an additional cost of $160,000.
 Hospitals are facing high readmission rates, higher mortality rates, and temporary closures due to infection outbreaks. Unsurprisingly, the public is alarmed, as headlines like“How Your Hospital Can Make You Sick” and “The Horror in Our Hospitals” do not inspire confidence.
Hospitals are facing high readmission rates, higher mortality rates, and temporary closures due to infection outbreaks. Unsurprisingly, the public is alarmed, as headlines like“How Your Hospital Can Make You Sick” and “The Horror in Our Hospitals” do not inspire confidence.
Most hospital acquired infections are preventable, and the CDC considers the epidemic a “winnable battle.” But winning will require radical change.Hospitals must become more diligent and more innovative to prevent the spread of infection.
“We are trying to solve problems of today with instruments of the past,” notes Ojan Assadian, M.D., an infectious disease consultant and president of the Austrian Society for Infection Control. “It is time to rethink our approach and combine existing strategies with new technology.”
How Infection Spreads at Hospitals
Crafting a new approach starts with recognizing just how easily infection is spread in the healthcare setting — and how inadequate current measures are.
Essentially, hospitals are facing a stealth crisis; the web of transmission routes is not only vast and complex but also invisible. As one microbiologist noted about lethal microbes: “Because we can’t see them, it is easy to forget that they are there.”Twenty-four hours a day, pathogens accumulate and travel throughout the hospital, as visitors, staff, and medical devices come and go.
Viral particles launched by a sneeze — or by a change of bed linens — hover in the air, to be inhaled by patients or to land on IV poles, wheelchairs, or stethoscopes. Pathogens deposited into a box of surgical gloves hitch a ride, via central line, to a patient’s bloodstream, or via catheter to the urinary tract. Bacteria travel from the bed rail of an infected patient to the hands of a nurse and from there, in any number of ways, to vulnerable patients.
Lethal microbes can proliferate even on intact skin, so healthcare workers’ hands can become contaminated after seemingly “clean” procedures such as taking a patient’s pulse or a temperature.Of course, the risk of transferring infection skyrockets when staff change wound dressings, handle a ventilator, or otherwise come in contact with blood, body fluids, or mucous membranes.
Humidifiers, supply carts, stretchers, glucometers, IV poles, portable computers, a doctor’s white coat or a necktie he absentmindedly touches before treating a patient — all can serve as vectors for transmission of pathogens as well.
Complicating matters, virulent microbes have remarkable staying power in the hospital environment. Clostridium difficile can last 5 months on hospital floors. Vancomycin-resistant enter ococci (VRE) can survive for up to 58 days on countertops. It’s no wonder patients have a 40% elevated risk of contracting an infection when they stay in rooms previously occupied by infected patients.
Given all this, any serious plan to control hospital acquired infections requires a combination of four strategies:
1. Bolstering antimicrobial stewardship programs
Though antibiotics are useless against bronchitis, the flu, and other viral infections, doctors routinely prescribe antibiotics for these conditions, fuelling the superbug crisis. Each year, more than 30% of U.S. oral antibiotic prescriptions, including half of all prescriptions for acute respiratory conditions, are unwarranted.Antibiotic misuse is pervasive in Europe as well, and hospitals worldwide are contributing to the problem.All hospitals must establish antimicrobial stewardship programs, led by infectious disease physicians who are on site or available remotely.
2. Improving hand hygiene among hospital staff
Hand hygiene compliance at hospitals is, in the words of the World Health Organization, “abysmally low” — typically under 40% and as low as 1% to 5%. Even when hand rub is readily available, dispensers are in working order, procedures are posted, and healthcare workers know they’re being observed, nurses and doctors often fail to rub their hands long enough, cover their wrists, remove gloves properly, and take numerous other critical preventive measures.It’s not that they’re lazy. They are focused on caring for patients and, as human beings, by nature engage in automatic, unconscious behaviours.Hospitals can nonetheless do better.
3. Improving surface cleaning protocols
A freshly cleaned hospital toilet cleaned may appear sparkling but, if not properly disinfected, remain teeming with pathogens. Fact is, hospital surface cleaning is inadequate.Hospitals must raise cleaning standards, using microfiber mopping systems,removing isolation-room curtains for cleaning, and properly disinfecting toilet handles, call buttons, tray tables, and other bacteria-laden surfaces. The most critical measure: replacing outsourced cleaning crews with staff crews.Studies show private crews tend to be underpaid and undertrained, feel less committed to the hospitals they service, perform their jobs with less diligence.The upshot:hospitals using outsourced cleaning have far higher rates of superbug infection.
4. Disinfecting the air
Vomiting, coughing, talking, even breathing can launch infectious microbes airborne. Mere conversation in the operating room can increase the airborne bacterial load and contaminate surgeons’ and nurses’ face masks. What’s more, pathogens are not just propelled into the air by sick patients; they are also carried into hospitals on the clothing and bodies of visitors and staff and swept via air currents into emergency entrances, lobbies, corridors, stairwells, and patient rooms.
It is clear that even vastly improved hand hygiene and surface cleaning will not suffice to halt the hospital infection crisis. Hospitals must deploy an additional line of defence against the spread of infection: disinfecting the air.
What’s more, healthcare facilities must go beyond HEPA filtration.These filters only trap— rather than kill — dangerous microbes, and pathogens caught in a HEPA filter can expose maintenance staff to infection. As more European hospitals are discovering, a more effective weapon is ultra-low-energy plasma technology.
 Novaerus portable air disinfection units useultra-low-energy plasma technology to reduce airborne viruses, bacteria, particulate, mould spores, VOCs, allergens and odours. The portable units are powerful, yet gentle. With no harmful by-products, they are safe for continued use around vulnerable populations.
Novaerus portable air disinfection units useultra-low-energy plasma technology to reduce airborne viruses, bacteria, particulate, mould spores, VOCs, allergens and odours. The portable units are powerful, yet gentle. With no harmful by-products, they are safe for continued use around vulnerable populations.
Novaerus recently launched their newest product, the Defend 1050. Designed for rapid remediation in large spaces and situations with high risk of infection, the Novaerus Defend 1050 (NV1050) uses patented ultra-low energy plasma technology combined with a triple-stage Camfil® filter system to provide a combined solution for air disinfection and particle removal. It kills pathogens and traps particulate to control infection.
“We created the Defend 1050 in response to a growing demand from our customers for a mobile, rapid remediation solution for airborne pathogens and VOCs in high-risk situations,” said Dr. Kevin Devlin, EVP of product at Novaerus. “As a problem solver, the Defend 1050 is the perfect complement to our filter-free units, the Protect 800 and Protect 200, which are designed to be operated continuously to maintain optimal indoor air quality.”
Novaerus technology has been independently tested and is trusted by hundreds of healthcare facilities around the world for safe, continuous, and effective air disinfection. For more information please visit www.novaerus.com.
The global crisis unleashed by superbugs demand a full-on attack. As infections become more difficult to treat, hospitals must work harder to destroy pathogens before they colonize filters, affix to healthcare workers’ hands, or settle on the lab coats, surgical instruments, bed rails, and other surfaces that serve as conveyor belts for infection. Traditional infection control protocols need reinforcement.Now, more than ever, we need to be looking at air disinfection to close the loop in infection control. Learn how Novaerus technology can augment current hygiene protocols to reduce infection.

















